Embolic Disease : FATAL CLOT
- Oct 20, 2022
- 4 min read
Embolic Disease : FATAL CLOT By Dr Rona Leonor
Venous thromboembolism (VTE) comprises deep vein thrombosis (DVT) and pulmonary embolism (PE ), it is one of the most frequent cardiovascular disease. The incidence of PE is approximately 60 -70 per 100, 000, and that of venous thrombosis approximately 124 per 100, 000 of the general population.1
The precise number of people affected by DVT/PE is unknown, although as many as 900,000 people could be affected (1 to 2 per 1,000) each year in the United States.Estimates suggest that 60,000-100,000 Americans die of DVT/PE (also called venous thromboembolism). 10 to 30% of people will die within one month of diagnosis. Sudden death is the first symptom in about one-quarter (25%) of people who have a PE. 11

Among people who have had a DVT, one-half will have long-term complications (post-thrombotic syndrome) such as swelling, pain, discoloration, and scaling in the affected limb. One-third (about 33%) of people with DVT/PE will have a recurrence within 10 years.
Image copied from www.carlossantosmdpa.com <http://www.carlossantosmdpa.com>
http://www.carlossantosmdpa.com/embolism.html
Approximately 5 to 8% of the U.S. population has one of several genetic risk factors, also known as inherited thrombophilias in which a genetic defect can be identified that increases the risk for thrombosis.11
In a study done by Woo-Suk Lee et al; among Asian patients the incidence of symptomatic PE was 0.01%. The incidence of overall DVT, proximal DVT and symptomatic DVT were 40.4%, 5.8% and 1.9% respectively. It was found out that there were no difference in incidence of symptomatic PE among Asian countries and no trends in changes of the incidence overtime.
In a study done by Bernardo et al in 2007 at the Philippine Heart Center, among the 106patients admitted at the medical and neurological ICU, 2.8% of the subjects developed proven DVT and PE.Seven out of the eight patients with either suspected or proven PE or DVT had Well’s score of more than or equal to two (more than or equal to moderate risk for DVT).
The pathophysiology of PE and DVT centers on thrombus formation, which can induce release of inflammatory mediators resulting in vasoconstriction, vascular obstruction and subsequently Right Ventricular (RV ) failure. The pressure overload can be a major cause of death among patients with PE. It decreases preload and Cardiac output, thereby causing hypotension.A silent PE can eventually develop into DVT.1
PE and DVT can result from multiple factors which includes age, previous history of VTE, malignancy, pregnancy, conditions of the heart -congenital or acquired, coagulation disorders, intake of hormone replacement therapy, obesity, major illness , recent surgery or trauma, immobilization, long haul air travel and other pathological lung conditions.
Symptoms of unexplained dyspnea, and sometimes chest pain either pleuritic or atypical are noted on PE. Tachycardia, tachypnea, low grade fever, tricuspid regurgitation and accentuated P2 can be also be seen during physical evaluation.
Edema is the most non specific symptom of DVT. Thrombus that involves the iliac bifurcation, the pelvic veins, or the vena cava produces produces leg edema that is usually bilateral rather than unilateral.3
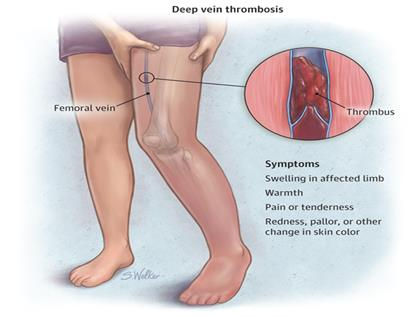
Image copied from the Journal of the American Medical Association (JAMA) http://jama.jamanetwork.com/article.aspx?articleid=2297171 Leg pain occurs in 50% of patients with DVT, but is entirely non specific. It can occur on dorsiflexion of the foot (Homans sign). When tenderness is presentit is usually confined to the calf muscles or along the course of the deep veins in the medial thigh. Clinical signs and symptoms of PE as the primary manifestation occur in 10% of patients with confirmed DVT.3
ECG, D dimer , Lung scanning, Compression Ultrasonography of the legs and echocardiography are some of the diagnostic tests used in in patients suspected of pulmonary embolism. Markers of RV dysfunction such as RV dilatation, hypokinesis or pressure overload on echocardiography can be seen. In contrast to the global hypokinesis seen in PAH patients with RV failure, PE patients may exhibit sparing of the RV apex with hypokinesis of the RV free wall and base -a finding termed the “McConnell sign.”4
Result fromCT angiography, BNP and troponin elevation are markers useful for risk stratification in acute Pulmonary embolism.
It can be classified as small to moderate, submassive and massive. Initial treatment is focus on restoration of blood flow. Anticoagulation is the mainstay of treatment.

Image copied from wikepidiahttps://en.wikipedia.org/wiki/Pulmonary_embolism

Image copied from Echocardiography in the diagnosis of Pulmonary Embolism. www. Cardioserv.net
Chest spiral HYPERLINK"https://en.wikipedia.org/wiki/CT_scan"CT scan with HYPERLINK"https://en.wikipedia.org/wiki/Radiocontrast"radiocontrast agent showing multiple filling defects both at the

Image copied from The American College of Emergency Physician website http://www.acep.org/Clinical---Practice-Management/Focus-On--Emergency-Ultrasound-For-Deep-Vein-Thrombosis/
In submassive and massive PE addition of thrombolysis or embolectomy or IVC filter are the options of treatment. The primary
objectives of the treatment of DVT are to prevent PE and reduce mortality and minimizes the risk of post thrombotic syndrome (PTS).
The immediate symptoms of DVT often resolve with anticoagulation alone, and the rationale for intervention is often reduction of the
75% long term risk of PTS .3
Hence, early detection and prompt treatment can aid to lower morbidity and mortality rate.
REFERENCE:
Pulmonary Embolism, Part I. epidemiology, risk factors, and risk stratification, pathophysiology, clinical presentation,
diagnosis and non thrombotic pulmonary embolism. Jan Belohlavek et al; Experimental and Clinical Cardiology, 2013
Spring: 18 (2): 129-138.
The Incidence of Pulmonary Embolism and Deep vein thrombosis After Knee Arthroplasty in Asians Remain Low: A meta
analysis. Woo-Suk Lee, et al; Clinical Orthopedic and Related researches. 2013 May; 47 (15): 1523-1532.
Deep venous thrombosis. KaushalpatelMd, et al; Medscape.
Acute Right Ventricular Failure in the Setting of Acute Pulmonary Embolism or Chronic Pulmonary Hypertension: A
Detailed Review of the Pathophysiology, Diagnosis, and Management ; Jennifer Cowger Matthews et al; Current
Cardiology review Feb 2008
2014 ESC Guidelines on the diagnosis and management of Acute Pulmonary embolism. European Heart Journal. Aug 29,
2014.
Echocardiography in the diagnosis of Pulmonary Embolism. www. Cardioserv.net
Central Line clot. www.psnet.ahrq.gov <http://www.psnet.ahrq.gov>
www.carlossantosmdpa.com <http://www.carlossantosmdpa.com>
NYC surgical associates. www.nycsurgical.net <http://www.nycsurgical.net>
Practices and Attitudes of Physicians on Deep Venous Thrombosis Prophylaxis Among Critically Ill Patients Admitted at The
Medical and Neurologic Intensive Care Units. Jasmin Melissa B. Bernardo MD et al, Division of Adult Cardiology. Phil
Heart Center J 2007; 13(2):113-118.
Venous thromboembolism: a public health concern.Michele G. Beckman, MPH,Am J Prev Med 2010;38(4S)S495-S501



Comments