PSVM VASCULAR CONVERGENCE CASE PROTOCOL
- Oct 10, 2022
- 4 min read
PSVM VASCULAR CONVERGENCE CASE PROTOCOL
June 8, 2016
“The Pretentious One”
Presentors: Charisse Mendoza Aldea,MD
Liezl L. Comia, MD
St. Luke’s Medical Center, Quezon City
Moderator: Laurencia G. Trinchera, MD
OBJECTIVES
To discuss the indications for use of thrombolytic therapy, its efficacy and outcome in Massive/Submassive Pulmonary Embolism
To discuss the dosage of thrombolytic therapy in elderly patients with Pulmonary Embolism
To discuss the diagnostic accuracy of conventional or age adjusted D- dimer cut off values in older patients with renal insufficiency. - To discuss the role of Pro BNP in the prognosis of Pulmonary Embolism.
PATIENT DATA
L.P., 81 year old female, Chinese, widow, Roman Catholic, retired, from Tondo, Manila
CHIEF COMPLAINT
dyspnea HISTORY OF PRESENT ILLNESS
40 days prior to admission, the patient complained of dizziness and episodic shortness of breath when walking 3 steps or more, but no dyspnea at rest. No consult or medications taken.
30 days prior to admission, the patient experienced dyspnea even at rest, which prompted her to seek consult. On the way to the hospital, she was observed by her daughter to be cyanotic. On admission, patient was noted to be in mild respiratory distress. Pertinent physical findings on examination include presence of rales in the left lung base and grade 1 edema in the right lower extremity. Diagnostic tests were requested, which revealed the following results: CXR: Significant clearing of prior
remote pneumonia with suggestive developing left basal fibrosis, atheromatous aorta and LV cardiomegaly; ABG showed uncorrected metabolic acidosis with underlying respiratory acidosis with uncorrected hypoxemia; 12 lead ECG showed normal sinus rhythm, old inferior and anteroseptal infarction; presence of leukocytosis with predominance of segmenters and thrombocytopenia on CBC and an elevated creatinine level at 2.26 mg/dl. The initial admitting diagnosis was of Acute Coronary Syndrome; Community Acquired Pneumonia, moderate risk; Acute renal failure secondary to acute cardiac event on top of Chronic kidney disease secondary to Hypertensive Nephrosclerosis vs Diabetic Nephropathy; Hypertensive Cardiovascular Disease; Diabetes Mellitus Type II and Dysplipidemia. She was started on the following medications: Cefepime, Azithromycin, Enoxaparin, Clopidogrel, Furosemide and Isosorbide dinitrate drip. Other diagnostic cardiac work up showed concentric LVH with normal LV index and increase RWT with normal wall motion and contractility with adequate systolic function EF 77%, normal LA, RA, RV, MPA and aortic root dimensions, thickened aortic and mitral valve cuspal margins with no restriction of motion, grade I decrease LV diastolic compliance with, Normal PAP on 2D echo and a normal Troponin T level. Due to the persistence of dyspneic episode and desaturation, patient was referred to pulmonary service with an impression of consolidation vs pleural effusion, left; R/O pulmonary embolism. D- dimer was done which showed an elevated level at 3.20 ug/ml. She was also observed to have progression of the bipedal edema hence venous duplex scan of the bilateral lower extremities was done which showed an acute deep venous thrombosis, totally occluding the right common femoral, proximal to distal femoral, peroneal and gastrocnemius veins; partially occluding the left common femoral, proximal to distal femoral and popliteal veins. She was given Apixaban 2.5mg once daily and Cilostazol 100mg daily. The patient was admitted for approximately 2 weeks and was eventually discharged with the use of Oxygen at home with Cilostazol, Apixaban, Linagliptin, Ketosteril, Isosorbide mononitrate, Metformin, Furosemide, Escitalopram, Ipratropium with Salbutamol and Cefixime as home medications.
14 days prior to admission, a day after discharge, she developed petechiae on her extremities, but without gross bleeding and was advised by her physician to stop Apixaban and Cilostazol.
9 days prior to admission, the patient again developed shortness of breath at rest and episode of desaturation (oxygen saturation of 88-89% at 1 lpm). She was noted to be tachypneic and tachycardic.
8 days prior to admission, due to the persistence of tachypnea and tachycardia, they called their physician and were advised to take Propranolol 10mg as needed for tachycardia. However on further observation, they noted that the patient developed hypotension, lowest BP of 80 palpatory, associated with cyanosis, hence were instructed by their physician to place patient in a Trendelenburg position. The physician made a home visit, advised to stop Propranolol. Chest Xray was requested to rule out Pulmonary Embolism but was not yet done. Dyspnea and tachycardia persisted.
7 days prior to admission, the patient was brought to the hospital due to persistence of symptoms. At the ER she was noted to be hypotensive, Dobutamine was started. She was started on LMWH. A repeat 2decho showed a normal LV cavity dimensions, normal wall thickness with flattened septum suggestive of RV volume and pressure overload and a dilated RV with hypokinesia. Repeat Venous Duplex Scan showed progression of thrombus distally. CT Angiogram of the pulmonary artery showed partial filling defect in both main right and left pulmonary arteries extending up to the interlobular pulmonary arteries with associated dilatation of both pulmonary arteries and trunk as well as right sided heart chamber dilatation and a wedge shaped high attenuation area in the superior segment of right lower lobe, antero-basal segment of left lower lobe and posterior segment of left upper lobe. Patient was then transferred to our institution for further management.
REVIEW OF SYSTEMS


PAST MEDICAL HISTORY
(+) Hypertension x 31 years -
- highest BP 180/90mmHg
- usual BP 130/70mmHg
- Medications:
o Losartan 50mg BID
o Metoprolol 50mg BID
(+) Type 2 Diabetes Mellitus x 8 years
- Medication:
o Metformin 500mg OD
(+) Dyslipidemia
- Medication:
o Sitagliptin 50mg OD
FAMILY HISTORY
(+) Diabetes Mellitus
PERSONAL AND SOCIAL HISTORY
Non smoker
Non alcohol beverage drinker
Denies illicit drug use
PHYSICAL EXAMINATION
General: conscious, coherent, afebrile, not in cardiorespiratory distress
Vital signs: BP: 130/80 HR 89 bpm RR 21/min Temp 36oC O2sat 100% on O2 2lpm
Skin: no active dermatoses, petechiae, rashes; (+) violaceous bruise noted on both antecubital fossa and on the site of IV line, right arm, dorsum of left hand and right groin
HEENT: anicteric sclerae, pink palpebral conjunctivae, pink nasal turbinates, supple neck, no cervical lymphadenopathies, no neck vein engorgement
Chest/Lungs: Symmetrical chest expansion, no retractions, bibasal rales left more than the right
Heart: Adynamic precordium, normal rate regular rhythm, no murmurs
Abdomen: (+) midline infraumbilical incision scar, soft, flabby, normoactive bowel sounds, non-tender, no masses noted
Extremities: ++ pulses on both right and left brachial, radial and dorsalis pedis arteries, no bipedal edema; (+) reticular veins on both lower extremities
IMPRESSION
1. Massive-Submassive Pulmonary Embolism
2. Subacute Deep Vein Thrombosis, S/P IVC filter insertion
3. Pulmonary Hypertension probably secondary to Pulmonary Embolism
4. Hypertensive Cardiovascular Disease
5. Type 2 Diabetes Mellitus
6. Acute Kidney Injury on top of Chronic Kidney Disease secondary to Hypertension vs DM Nephropathy
7. Dyslipidemia
LABORATORIES
















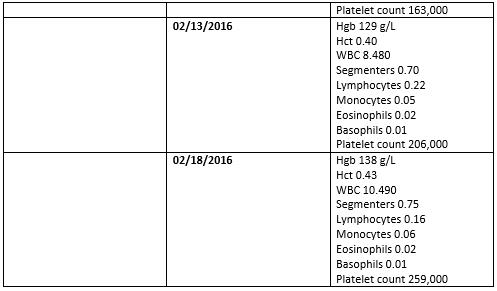



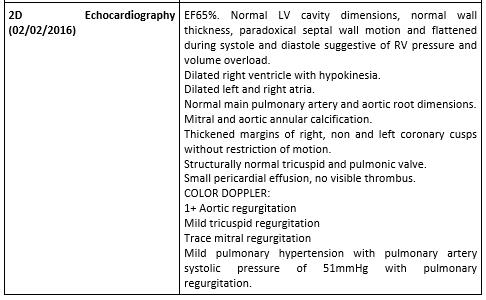














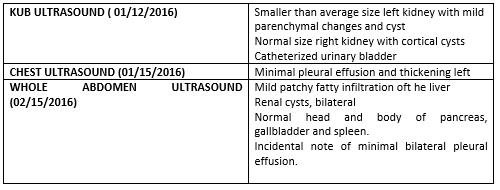
Comments